Vitamin D and Testosterone Levels: Can Vitamin D Increase Testosterone?
Vitamin D is a vital nutrient and hormone that influences many areas of our health, including bones, muscle movement, immune system functions, and neuro connections with the brain. Receptors and metabolizing enzymes for vitamin D are expressed in Sertoli and Leydig cells, spermatozoa, and germ and epithelial cells in the male reproductive tract, which is why it may also influence testosterone (T) levels.
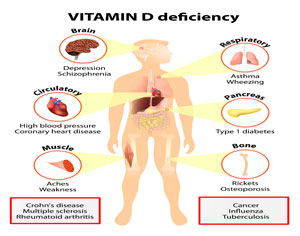
Vitamin D deficiency may or may not lead to testosterone deficiency. The research on this subject is currently inclusive. Some reports show a correlation between the two, especially when age and obesity are in the mix. Other reports show little to no difference in testosterone levels from vitamin D supplementation.
Vitamin D deficiency and low testosterone can significantly affect men’s health. Men with low vitamin D levels are more likely to suffer from frequent illness, weakening bones, dental abnormalities, depression, and a higher risk of developing multiple sclerosis (MS).
Many males do not realize that testosterone deficiency can increase the risk of developing or worsening cardiovascular disease, metabolic syndrome, type 2 diabetes, and atherosclerotic disease of the aorta. Low testosterone may also increase the risk of prostate and other aggressive variants of cancer.
What Is Vitamin D and How Important Is It?
Vitamin D is an essential nutrient that the body cannot produce without outside help. Sunlight exposure is the most common method of helping your body produce vitamin D. Supplements are also available for those with vitamin D deficiency.
While it is also a hormone, its role as a vitamin is undeniable, as it makes the body better able to absorb critical nutrients such as phosphorus and calcium, which are crucial for healthy bones. That is why so many products, especially those for children, are fortified with vitamin D.
Vitamin D helps support the blood vessels, protecting against lipid buildup in the arteries, arterial stiffening, and vascular dysfunction. Research has linked increased heart attack, heart disease, and ischemic stroke risk to lower vitamin D levels. It is also crucial for bone health, immunity, and maintaining nerve connections to the brain.
Aside from the testes, where most of the testosterone production occurs, androgen production, activation, and metabolism also occur in the skin, where vitamin D synthesis starts following exposure to sunlight.
It takes, on average, 15 minutes of sun exposure daily for the body to produce adequate vitamin D. That time frame changes based on time of year and geographical location. Individuals closest to the equator receive the best vitamin D exposure, and those living further away, especially during the winter, receive the least and require more outdoor time in the sun.
The reduced intensity of the sun’s rays in the winter may inhibit people living in the northern part of the US from manufacturing vitamin D, no matter how long they spend outside. Supplementation may be necessary, especially for older adults whose skin does not produce vitamin D, as well as younger adults.
In addition to sunlight, the other sources of vitamin D include:
- Vitamin D supplements (drops, pills, tablets, capsules). There are two forms of vitamin D, Vitamin D2 (plant form) and vitamin D3 (produced by humans and animals)
Vitamin D3 is the most recommended form for supplementation, as it is the type made by our bodies, although both forms are absorbable by the small intestine
- Vitamin D-fortified bread, juice, cereal, milk, yogurt
- Foods: sardines, salmon, trout, tuna, mackerel, liver, eggs, cheese, white mushrooms
- Fish liver oils
Check the labels when purchasing the foods listed above to ensure they are fortified with vitamin D.
Are your vitamin D levels low?
The table below shows blood levels for serum 25-Hydroxyvitamin D [25(OH)D], the indicator doctors use to measure vitamin D levels:
| Vitamin D Health Status | Nanogram per milliliter ng/mL | Nanomoles per liter nmol/L |
| Deficient levels of vitamin D | <12 | <30 |
| Inadequate for overall and bone health | 12 to <20 | 30 to <50 |
| Adequate vitamin D levels | ≥20 | ≥50 |
| High levels with possible adverse effects | >50 | >125 |
It is essential to point out that vitamin D and testosterone can severely impact the body when their levels are low, as highlighted in the chart below:
| Symptom | Vitamin D Deficiency | Testosterone Deficiency |
| Bone loss, pain, osteoporosis, and osteomalacia risk | X | X |
| Muscle weakness, pain, or loss | X | X |
| Depression | X | X |
| Increased multiple sclerosis risk | X | |
| Fatigue and lack of endurance | X | X |
| Trouble sleeping | X | X |
| Hair loss | X | X |
| More frequent illness/reduced immune functions | X | |
| Loss of appetite | X | |
| Pale skin | X | |
| Reduced sex drive | X | |
| Obesity/weight gain | X | |
| Erectile dysfunction | X | |
| Testicular shrinkage | X | |
| Hot flashes | X | |
| Trouble with concentration, decision-making, and memory | X | |
| Breast tissue enlargement (gynecomastia) | X | |
| Reduced red blood cell production | X | |
| Decreased exercise results | X | |
| Elevated LDL and total cholesterol | X | X |
| High blood pressure | X | X |
| Increased inflammation | X | X |
| Glucose metabolism | X | X |
| Rickets | X | |
| Pins and needles feeling in feet or hands | X |
It is easy to see that being deficient in vitamin D or testosterone can cause significant health problems for adults.
The most common causes of vitamin D deficiency include:
- Lack of sun exposure
- Family history of vitamin D deficiency
- Malnutrition
- Darker pigmented skin
- Liver or kidney failure, which decreases vitamin D processing
- Lymphoma and some other cancer types
- Some medications
People with the following conditions may have trouble absorbing vitamin D, including:
- Celiac disease
- Cystic fibrosis
- Inflammatory bowel disease (ulcerative colitis and Crohn’s disease
- Small intestine resection surgery
- Bariatric weight loss surgery
- Exocrine pancreatic insufficiency
Can vitamin D deficiency cause low T?
Studies are conflicting on this subject. Some research points to vitamin D deficiency reducing testosterone production, especially in obese men. Other studies do not find an association. Whether or not vitamin D influences T levels, one fact is inevitable – keeping these levels in proper balance is crucial.
Does Vitamin D Increase Testosterone?
Obesity and aging are two causes of low testosterone, so examining methods of increasing testosterone is crucial. Vitamin D deficiency is often present when T levels are low, especially in younger men who are overweight. However, there is no consensus at this time that vitamin D supplementation can increase T levels. It only shows that morbidly overweight men have low T and D levels, which are both effects of obesity.
The report states that several epidemiological studies show vitamin D deficiency is connected to obesity, yet there is no significant impact on bone metabolism or bone mineral density. Vitamin D deficiency was linked to other issues due to its importance in insulin sensitivity, lipid accumulation, inflammatory signaling in adipose tissue, reduced T levels, and increased hypogonadism risk. *Note this means link – not cause.
A study from Germany on 200 overweight healthy men showed that vitamin D3 doses of 3,333 IU daily did not support weight loss but did decrease triglycerides and cytokine TNF-alpha levels slightly. There was also a slight increase in bad LDL cholesterol and a small increase in testosterone levels. Total T levels rose by an average of 3 nmol/liter after 12 months.
A 2021 meta-analysis of 18 studies showed a slight but positive association between vitamin D and total testosterone levels. These reviews showed variable differences, such as one suggesting that low bioavailable testosterone was only significant for men with extremely low vitamin D levels and that the difference was relatively small.
Other studies show no significant differences in men receiving vitamin D and T levels. Body mass index (BMI) may play a more significant role in the relationship between D and testosterone, although more research is necessary as the ultimate findings are inconclusive.
Other studies do not support this association, and vitamin D supplementation has not been shown to increase serum testosterone levels.
There is no difference in how the various types of vitamin D affect T levels. Vitamin D3, derived from animals, may raise D levels in the bloodstream longer than vitamin D2, which is plant-derived.
How much vitamin D should you take to increase testosterone?
There are no recommendations for taking vitamin D to increase testosterone levels. The best method for boosting low T is testosterone replacement therapy.
However, unless you get enough vitamin D from sunlight and food, the vitamin D daily recommended dosage is:
- 600 IU (15 mcg) for adults under 70
- 800 IU (20 mcg) for adults over 70
Too much vitamin D can increase the risk of high calcium levels and kidney stones. Unless medically directed, do not take more than 4,000 IU daily.
Speaking with a hormone specialist is the best way to ensure you do everything possible to keep your testosterone and vitamin D levels balanced to protect your body and health.
- Effect of vitamin D supplementation on testosterone levels in men.Pilz S1, Frisch S, Koertke H, Kuhn J, Dreier J, Obermayer-Pietsch B, Wehr E, Zittermann A.Horm Metab Res. 2011 Mar;43(3):223-5
- Vitamin D and Testosterone in Healthy Men: A Randomized Controlled Trial. Elisabeth Lerchbaum, Stefan Pilz, Barbara Obermayer-PietschPublished in The Journal of clinical endocrinology 2017