Hormone Replacement Therapy and Hysterectomy
Discussing hormone replacement therapy and hysterectomy options with women can bring on many emotions. First, hormone replacement therapy (HRT) is a confusing topic as research provides an abundance of pros and cons on the subject. Second, the decision to get a hysterectomy and possibly also an oophorectomy is a personal one and can signal the end of a woman’s ability to conceive and carry a child. For many women, the decision is based on medical reasons, which may also increase stress.
Do I need to take HRT after hysterectomy?
The decision about taking HRT after hysterectomy is one to make in conjunction with a doctor who specializes in women’s hormone balancing. Each woman is unique, as is her circumstances. In this report, we will look at the pros and cons of various types of hormone treatments available after a hysterectomy.
What Is the Difference Between a Hysterectomy and an Oophorectomy?
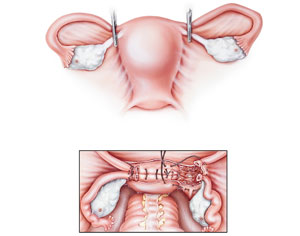
A woman’s abdomen contains both her uterus and ovaries. A hysterectomy is the surgical removal of the uterus but leaves the ovaries intact. In a total or bilateral oophorectomy, the doctor also removes both ovaries. A unilateral oophorectomy removes only one ovary, leaving the other. A woman may not experience any menopausal symptoms as long as she still has one ovary producing hormones.
When the ovaries are also removed during a total abdominal hysterectomy, and HRT is recommended, it is because the body often enters what is called “surgical menopause.” The ovaries are the producers of hormones that include progesterone, testosterone, and estrogen.
Following ovarian removal, these hormone levels plummet rapidly. A woman may experience many of the symptoms of menopause right away.
With prescription HRT, hysterectomy, and oophorectomy, responses to surgical menopause are prevented or significantly lessened. An oophorectomy and hysterectomy without HRT can increase the risk of a woman suffering from hot flashes, sleep disturbances, night sweats, mood changes, cognitive decline, cardiovascular disease, and weakening bones.
Hormone replacement therapy and hysterectomy is a personal decision to discuss with a qualified doctor.
What Happens to a Woman’s Hormone Levels After a Hysterectomy?
Because a hysterectomy only removes a woman’s uterus, it does not alter hormone levels. Leaving the ovaries intact allows for natural hormone production to continue. Some females may experience menopause a few years earlier than they would have without a hysterectomy.
As we continue our review of hormone replacement therapy and hysterectomy, we begin with a look at the changes that accompany both a hysterectomy and oophorectomy:
- Hysterectomy Changes – with a hysterectomy, the uterus is removed from the woman’s body. A woman may opt to have her uterus removed if she suffers from uterine fibroids that cause pain and heavy periods, uterine prolapse, endometriosis pelvic pain, or uterine cancer. Without a uterus, a woman will not be able to conceive and carry a fetus. She will no longer have her monthly period. However, it may be possible to harvest a woman’s eggs from her ovaries if she would like to donate them or have a baby carried by a surrogate.
- Oophorectomy Changes – with the removal of the ovaries, the production of critical hormone levels declines. Although the adrenal glands and peripheral tissues continue to make small amounts of these hormones, it may not be enough to support physiological functions. A woman’s body no longer produces eggs without the ovaries.
Do you need HRT after hysterectomy?
With only the uterus removed, the ovaries still produce hormones, so HRT may not be necessary.
Do I need HRT after a complete hysterectomy and oophorectomy?
The answer here often depends on age and symptoms. Women who are over 50 are at a stage in life where natural menopause usually occurs. If they have no symptoms, or the symptoms of menopause are not severe, they may choose not to undergo HRT. It is recommended that women under age 50 go on HRT for a while to protect their bones, heart, and brain.
What Types of Hormone Therapies Are Available After a Hysterectomy?
Most women automatically assume the only types of HRT after hysterectomy are estrogen and progesterone. However, there are some other options, as shown below:
- Estrogen – women who have both a hysterectomy and oophorectomy often receive only estrogen replacement therapy (ERT). Estrogen is crucial for maintaining healthy brain functions and bone density.
- Progesterone – the term progestogen not only describes progesterone, but also progestin, the synthetic form of progesterone. Hormone doctors prefer natural (bioidentical) progesterone over progestin as it carries fewer side effects. Women who have their ovaries removed but still retain their uterus must receive both estrogen and progesterone to reduce the risk of uterine cancer.
- Testosterone – because testosterone is a precursor hormone to estradiol (estrogen), hormone specialists often prefer this form of bioidentical hormone treatment as it can also increase estrogen levels more safely than ERT. Research shows testosterone replacement therapy (TRT) as a safe way to improve muscle mass, sexual function, cognitive performance, mood, and physical functions.
- Human Growth Hormone – HGH has significant actions in the ovaries and with follicular development and sensitivity to aid fertility. In menopausal women, HGH acts on the adrenal glands to increase plasma DHEAS levels. DHEA is a precursor hormone to testosterone production, which subsequently converts via aromatase into estradiol. HGH supports sexual functions, metabolism, bone, muscles, heart health, and brain functions. In this way, HGH has a direct and indirect action on menopausal symptoms.
One thing to know about hormone replacement therapy and hysterectomy is that many women who receive ERT following their surgery continue to experience symptoms of testosterone deficiency. The benefits of taking HRT after hysterectomy that is targeted to the body’s needs via comprehensive blood analysis can make a tremendous difference in health and well-being.
How Long Can I Stay on Hormone Replacement Therapy After a Hysterectomy?
When asking, how long should you stay on HRT after hysterectomy, the goal of any hormone treatment is to use it for the shortest time possible. Although many forms of bioidentical hormone replacement therapy and hysterectomy treatment are safe, the purpose of HRT is to reduce symptoms of menopause and restore proper balance to the body. Many women who have an oophorectomy before age 50 take HRT only up until they reach the age of natural menopause – around 51 years.
Age is also an issue with HRT following hysterectomy as well as menopausal treatment overall. In one study, estrogen use did not increase breast cancer risk in women who took it for 10 years following oophorectomy. Both testosterone and HGH therapies are deemed safe for long-term use under a doctor’s care. Yearly blood tests monitor hormone levels.
What Are the Risks of Hormone Replacement Therapy?
We will now look at the risks associated with hormone replacement therapy and hysterectomy:
- Estrogen – oral estrogen may increase the risk of blood clots and ovarian cancer. Breast cancer risk does not increase with estrogen alone unless it is in use for over 6 years.
- Progesterone/Progestin – synthetic progestin with estrogen may increase heart attack and breast cancer risk.
- Testosterone – high levels of testosterone could increase the risk of acne, oily skin, clitoral enlargement, changes in hair growth, and deepening of the voice. Serious side effects are rarely seen with TRT.
- Human Growth Hormone – HGH therapy is deemed safe for those adults with growth hormone deficiency. The most likely issues if growth hormone levels get too high are insulin sensitivity, type 2 diabetes, acromegaly, carpal tunnel syndrome, joint pain, and edema.
Some women begin HRT for menopause symptoms only to have a hysterectomy or oophorectomy later. Stopping HRT before hysterectomy is not necessary and can have benefits if surgical menopause is likely due to an oophorectomy. As with any treatment, it is essential to discuss all options with your doctor.
How Do I Find Out if Hormone Replacement Therapy Is Right for Me?
Should you take HRT after a hysterectomy and oophorectomy? The best person to ask is a hormone specialist who can run the appropriate blood tests to measure your hormone levels.
What is the best HRT to take after hysterectomy?
Hormone therapy is not one-size-fits-all. It should always be customized to individual needs. Some gynecologists routinely prescribe estrogen ERT to women following an oophorectomy and hysterectomy.
We strongly recommend having hormone levels checked if any symptoms, including weight gain or changes in mood or sex drive, occur. Estrogen may not be the right choice for you. Personalized HRT is always the best option – especially when you can receive bioidentical rather than synthetic hormones.
For more information about hormone replacement therapy and hysterectomy treatment options, please contact National HRT for a free, confidential phone consultation.